A Protocol for Adapting MAPNET Battery for Pediatric Psychosis:
Bernalyn Ruiz-Yu, PhD (1,2), Peter Bachman, PhD (1,2), Benjamin Mills, BS (1), Joseph Gonzalez-Heydrich, MD (1,2)
1. Boston Children's Hospital
2. Harvard Medical School
Background: Schizophrenia Spectrum Disorders (SSD) are among the most debilitating psychiatric illnesses, characterized by positive, negative, and cognitive symptoms. Coordinated Specialty Care (CSC) is the gold-standard treatment model and includes individualized medication, individual resiliency training (IRT), supported employment/education (SEE), and family education (FE). Early-onset SSD (EOSSD), defined by onset before age 18, is rare and typically associated with poorer prognosis and limited treatment options. To date, CSC for psychosis has not been systematically studied in pediatric populations. However, meta-analytic research on wraparound services for children with serious emotional disorders suggests that team-based, community-focused models can yield significant benefits, particularly in maintaining youth in community settings and reducing costs. Establishing efficacy of pediatric-adapted CSC requires first identifying appropriate outcome measures. The Developmental Neuropsychiatry & Psychosis (DNP) team at Boston Children’s Hospital is adapting existing assessment batteries for use in pediatric SSD.
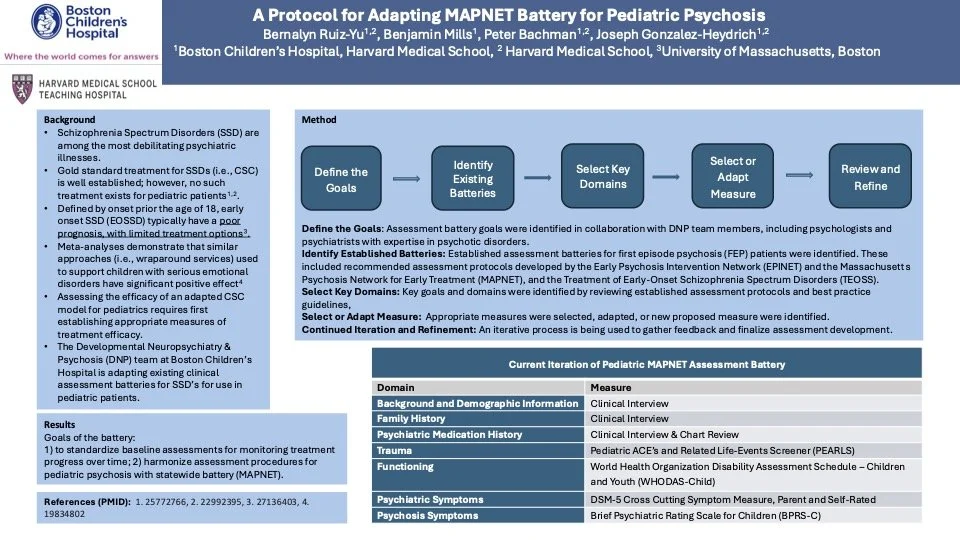
Method: Assessment battery goals were identified in collaboration with psychologists and psychiatrists specializing in psychotic disorders. Existing first-episode psychosis protocols, including those recommended by the Early Psychosis Intervention Network (EPINET) and Massachusetts Psychosis Network for Early Treatment (MAPNET), were reviewed. Domains and measures were selected or adapted through an iterative process to align pediatric needs with statewide standards.
Results: Battery goals were defined as: (1) standardizing baseline assessments for longitudinal treatment monitoring, and (2) harmonizing pediatric psychosis assessments with MAPNET procedures. Key domains and proposed measures include demographics, family psychiatric history, psychotropic medication history, trauma, functioning, trauma (Pediatric ACE’s and Related Life-events Screener (PEARLS)), functioning (World Health Organization Disability Assessment Schedule – Children and Youth (WHODAS-Child)), psychiatric symptoms (DSM-5 Cross Cutting Symptom Measure, parent and self-rated), and psychosis symptoms (Brief Psychiatric Rating Scale for Children-(BPRS-C)).
Discussion: Establishing progress-monitoring protocols is essential to developing gold-standard care for pediatric psychosis. The DNP team’s adapted assessment battery and initial EOSSD sample data will be presented.