Our Mission
MAPNET's mission is to offer technical assistance on best practices in first episode psychosis (FEP) treatment to service providers throughout the state of MA. Read on to understand the history and importance of this project.
Scope of the Problem
Psychotic disorders typically emerge in late adolescence and early adulthood, have a lifetime prevalence of 3%, often lead to frequent hospitalization, and derail functioning in school, career, and social relationships. There is accumulating evidence that early identification and intervention (EI) can promote recovery and minimize the disability caused by these disorders.
Why early intervention (EI) in psychosis?
EI can substantially reduce relapse, disability and chronicity.
Delays of up to 2 years are seen between the onset of psychosis and initiation of treatment (Perkins et al., 2005; PMID 16199825); such delays are associated with poor outcome (Keshavan et al 2003; PMID14989413) and disengagement from the social world and other socially and biologically maladaptive processes (e.g., weight gain, loss of work or interrupted schooling). Stigma, limited mental health training, and negative attitudes about psychiatric treatment interfere with help seeking and delay appropriate diagnoses. The “duration of untreated psychosis” (DUP) can be reduced by early referral and treatment of youth in the early stages of psychotic illness, and such reductions improve long term outcome (Hegelstad et al., 2012; PMID 22407080).
EI may protect brain development.
The brain is more “plastic” (better able to adapt) during adolescence and early adulthood. This period of development is also critical to maturation of cognitive, emotional, and social functioning. The emergence of a psychotic disorder is often associated with decline in brain structure and function, as well as deterioration (or failure of normal growth) of social, academic, and vocational functioning, as well as overall quality of life. The timing of therapeutic intervention may be critical to altering brain, cognitive, and functional outcomes and preventing long-term disability.
EI can save lives.
Suicide risk is high in early psychosis. In schizophrenia, nearly 50% of all suicides occur in the first 5 years of illness. Many attempt suicide prior to treatment. Specialized EP treatment programs decrease suicide risk (Addington et al., 2004; PMID 14725592). Substance abuse, psychosis, and mood disorders underlie such risk. The risk of violence in mental illnesses such as schizophrenia is highest for those with no, delayed, or inadequate treatment and comorbid substance use disorders during the initial episode, and might be mitigated with early treatment.
Approaches to EI in psychotic disorders
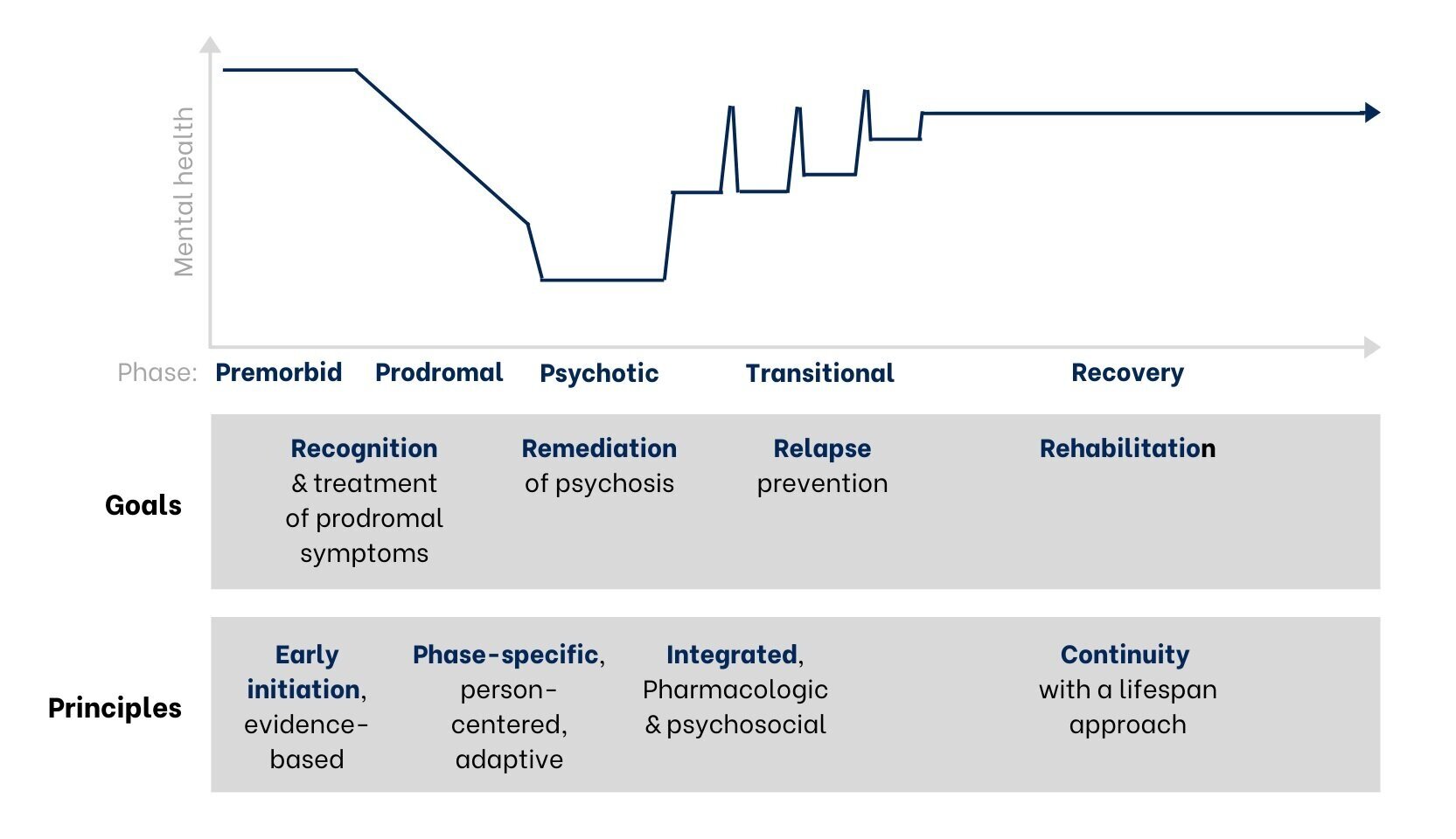
The graph below shows the phases of early psychosis and key principles of treatment. At the earliest signs of psychosis, our focus is to provide Early & Evidence-Based treatment. Ongoing care should be Phase-Specific based on an individual’s needs and situation, with the treatment approach Integrated across both a person’s development over time (longitudinally) and across their medical, therapeutic, and social contexts (cross-sectionally). Lastly, Continuity of Care must be maintained. This is known as the “EPIC” treatment model.
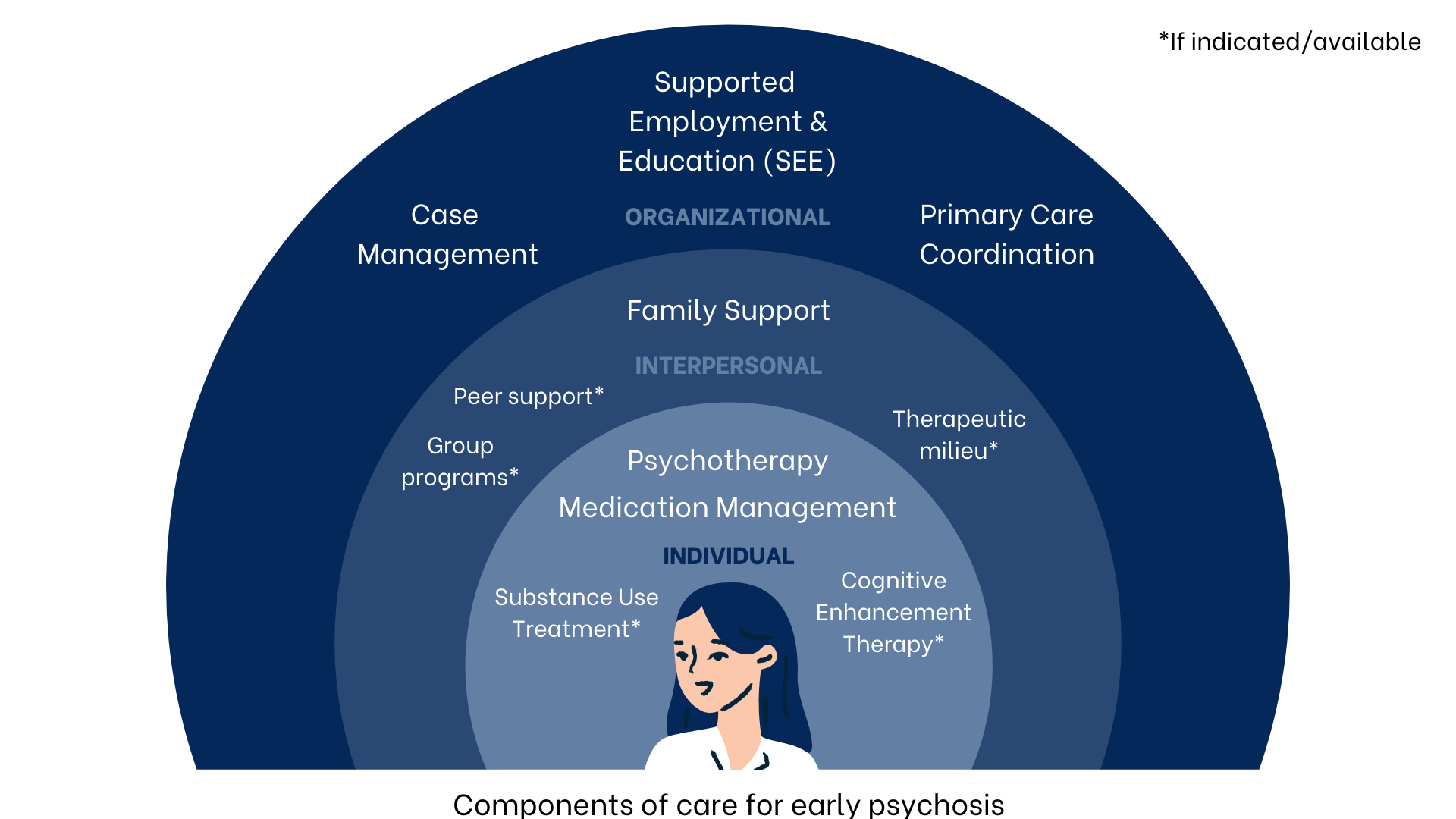
Elements of EI include psychotherapy, medication management, education and support for families, individualized support with school or work, and case management (ex. assistance with basic needs such as transportation and housing). While there are many different ways to implement evidence-based care for psychosis, the first priority is to limit the amount of time that psychosis is untreated by quickly and effectively engaging clients in care. Therefore, finding clients early in their illness and offering services that promote engagement and retention is a priority.
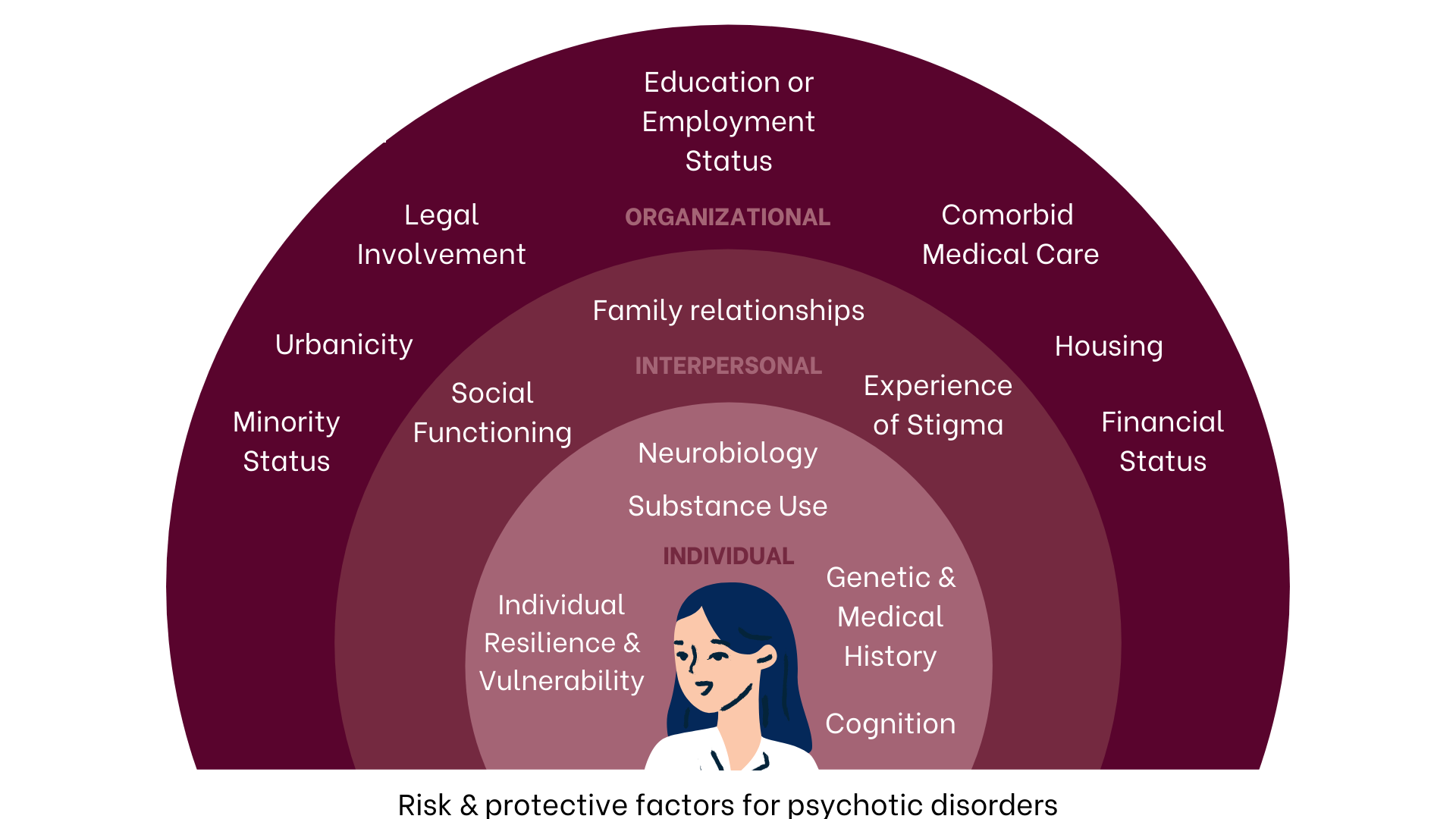
Whole-person care is similarly a priority; psychosis is rarely the only problem in a teen or young adult’s life, and other issues such as substance use, housing instability, loneliness, racism, trauma, family conflict, sexual health, or uncertainty about school or work may be just as pressing for someone entering a FEP program. The approach to treatment must be individualized based on this “whole-person” conceptualization of a person’s illness, as pictured below. Lastly, all treatment should be recovery-oriented, with the goal of helping an individual meet their personal recovery goals rather than simply reducing or controlling symptoms.
Specialized multi-element EI programs such as the RAISE Connection (New York) and STEP (New Haven, CT) programs have been shown to improve symptoms and quality of life and reduce re-hospitalizaitons better than standard outpatient care.* Collectively called “coordinated specialty care”, these programs provide many of the services outlined above in an integrated outpatient setting.
Interventions such as cognitive-behavioral therapy (CBT) and cognitive enhancement therapy (CET) also show promise in early intervention studies; effective care models may additionally include peer support, group programs, and integrated medical and substance abuse services. In Massachusetts, we have prioritized a comprehensive approach to EI that uses these evidence-based service elements to meet the needs and interests of local settings (Kline & Keshavan, 2017).
*Kane et al., 2015 [PMID 26481174]; Srihari et al 2015 [PMID 25639994]
Our role is to support top-quality FEP care in Massachusetts.
A community of well-trained professionals in Massachusetts is key to develop and implement these services at at all levels of care. The MAPNET team has the knowledge and skills to train providers across the state in evidence-based, person-centered care models. Through our learning collaboratives, consultations, and workforce development programs, we reach providers looking to develop and maintain clinical skills in EI. Our goal is to engage each FEP program individually, while also encouraging community and collaboration, in a “hub-and-spokes” model.