The Relationship Between Childhood Trauma, Abnormal Visual Experiences, and Visual Perceptual Functions in Young Individuals
Doğa Öge (1), Jonah Loshin (1), Nathaniel Weiler (1), Elif Ozan (1), Grace Owens (1), Zachary Milman (1), Dost Öngür (1), Halide Bilge Türközer (1)
1. McLean Hospital
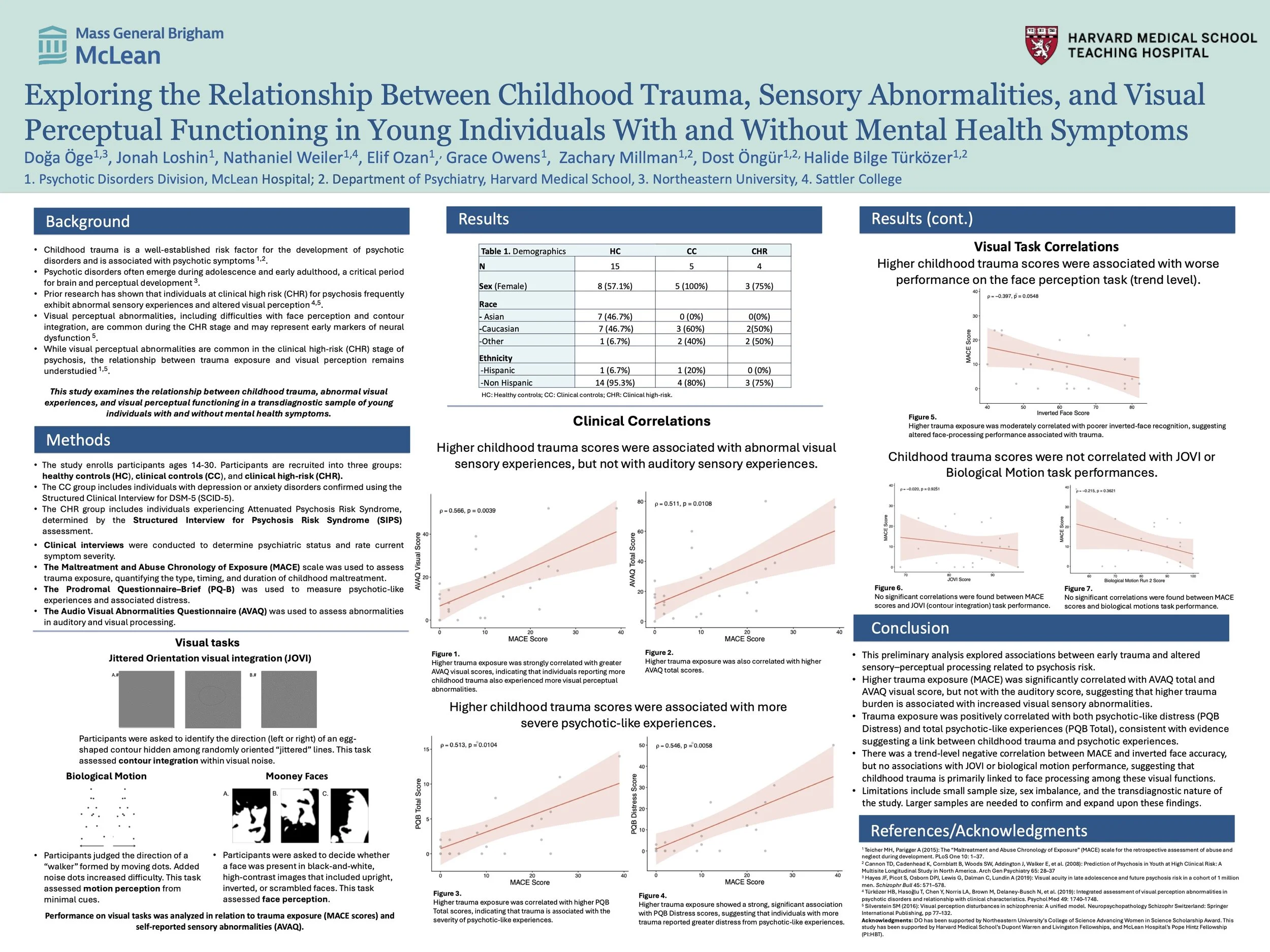
Background: Childhood trauma is a well-established risk factor for the development of psychotic disorders and is associated with psychotic symptoms. While visual perceptual abnormalities are common in the clinical high-risk (CHR) stage of psychosis, the relationship between trauma exposure and visual perception remains understudied. This study examines the relationship between childhood trauma, abnormal visual experiences, and visual perceptual functioning in a transdiagnostic sample of young individuals with and without mental health symptoms.
Methods: Participants (ages 15–30, N = 19) included healthy controls (n = 11), clinical controls with depression or anxiety (n = 5), and individuals at clinical high risk for psychosis (n = 3). Trauma exposure was assessed using the Maltreatment and Abuse Chronology of Exposure (MACE) scale. Abnormal sensory experiences were assessed using the Audio-Visual Abnormalities Questionnaire (AVAQ). Visual processing was evaluated with the Mooney Faces Task (upright, inverted, and scrambled conditions) and the Jittered Orientation Visual Integration (JOVI) task, which measures contour integration. Spearman correlations were conducted between trauma and perceptual outcomes.
Results: MACE scores were positively associated with AVAQ visual subscores at a trend level (ρ = 0.441, p = 0.059). Higher MACE scores were significantly associated with face perception accuracy. Greater trauma burden was related to better performance on detecting upright faces (ρ = 0.578, p = 0.0095), but poorer performance on inverted faces (ρ = –0.507, p = 0.027). No significant associations were observed between MACE scores and JOVI performance (ρ = 0.156, p = 0.52).
Conclusions: In this preliminary analysis, childhood trauma was significantly associated with alterations in face perception and showed a trend-level association with abnormal visual experiences, but not with contour integration. These findings suggest that trauma-related developmental disruptions might be linked to visual processing deficits in psychosis. These relationships should be further examined in larger samples.